Tel:+8618231198596

News
 CONTACT
CONTACT
 CONTACT
CONTACT
- Linkman:Linda Yao
- Tel: +8618231198596
- Email:linda.yao@dcpharma.cn
- Linkman:CHARLES.WANG
- Department:Overseas
- Tel: 0086 0311-85537378 0086 0311-85539701
News
Nisin of action involves disrupting bacterial cell wall synthesis.
TIME:2024-08-08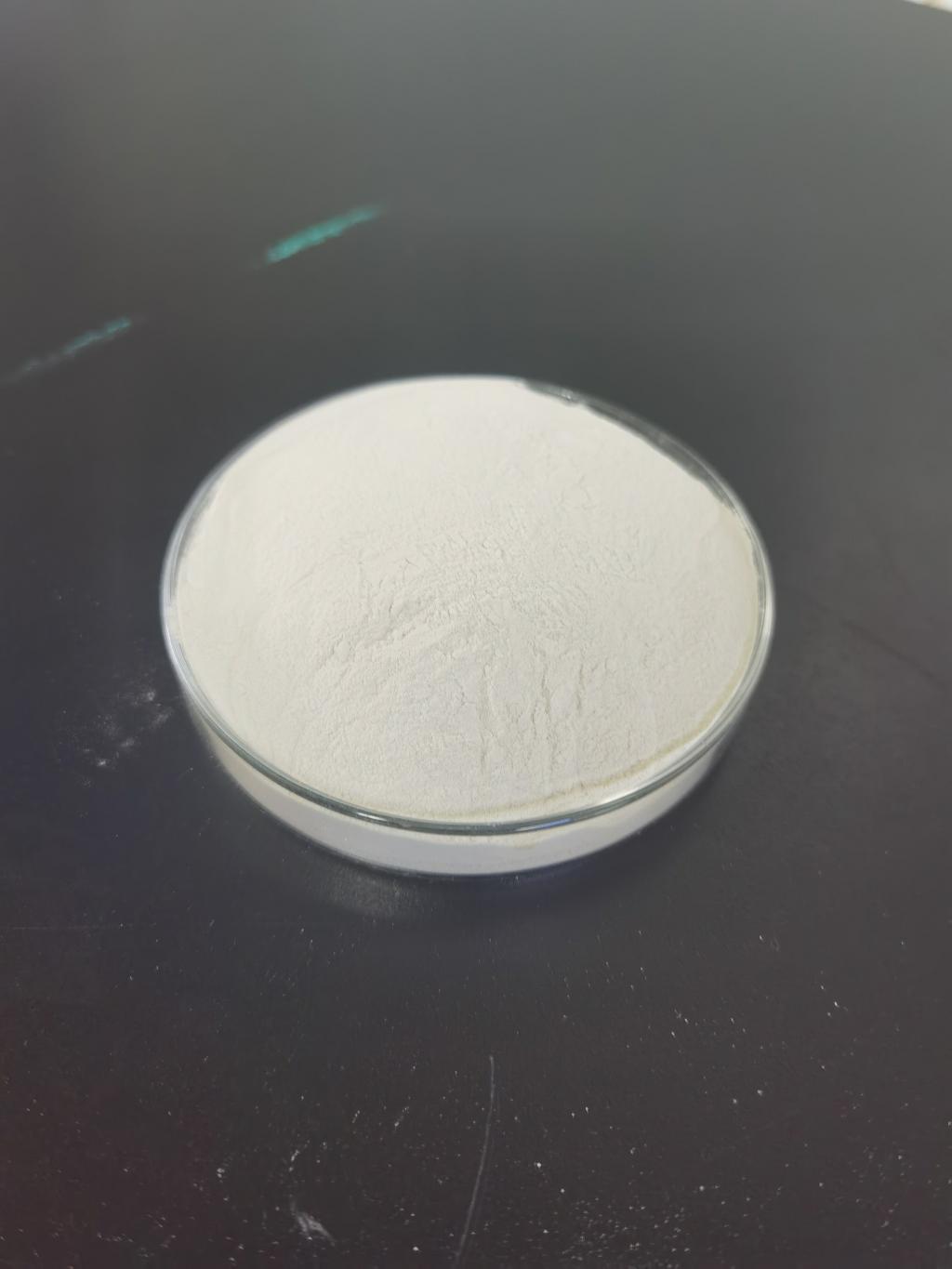
Mechanism of Action: Disrupting Cell Wall Synthesis
The bacterial cell wall is a critical structure that maintains the integrity and shape of the cell, protects it from osmotic pressure, and provides a barrier against environmental threats. The primary component of the bacterial cell wall in Gram-positive bacteria is peptidoglycan, a polymer consisting of sugars and amino acids. The synthesis of peptidoglycan is an essential process for bacterial growth and survival.
Nisin disrupts bacterial cell wall synthesis through a multi-step process:
Binding to Lipid II: Lipid II is a crucial precursor in the synthesis of peptidoglycan. It acts as a carrier molecule that transports peptidoglycan subunits across the bacterial cell membrane to the site of cell wall assembly. Nisin binds with high affinity to lipid II, effectively sequestering it and preventing its incorporation into the growing cell wall. This binding is facilitated by the unique structure of nisin, which allows it to interact specifically with lipid II molecules.
Pore Formation: In addition to inhibiting cell wall synthesis, nisin also forms pores in the bacterial cell membrane. The binding of nisin to lipid II facilitates the insertion of nisin into the cell membrane, where it aggregates to form pores. These pores disrupt the membrane's integrity, leading to leakage of essential ions and molecules, which ultimately results in cell death.
Dual Mechanism of Action: The combination of inhibiting cell wall synthesis and forming pores in the membrane makes nisin exceptionally effective. This dual mechanism of action ensures that nisin not only prevents the bacteria from growing but also rapidly kills the cells by compromising their membrane integrity.
Effectiveness Against Bacterial Pathogens
Nisin's ability to disrupt bacterial cell wall synthesis and form pores in the membrane makes it effective against a wide range of Gram-positive bacteria. Some notable examples include:
Staphylococcus aureus: S. aureus is a major cause of hospital-acquired infections and is known for its ability to develop resistance to multiple antibiotics. Nisin has shown potent activity against both methicillin-sensitive and methicillin-resistant strains of S. aureus (MRSA), making it a valuable option for treating infections caused by this pathogen.
Streptococcus pneumoniae: This bacterium is a leading cause of pneumonia, meningitis, and sepsis. Nisin's activity against S. pneumoniae highlights its potential for treating respiratory and invasive infections, particularly in the face of rising penicillin resistance.
Clostridium difficile: C. difficile is responsible for severe gastrointestinal infections, especially in individuals undergoing antibiotic therapy. Nisin has demonstrated efficacy against C. difficile, offering a potential alternative treatment for this challenging infection.
Listeria monocytogenes: Known for causing foodborne illnesses, L. monocytogenes can be particularly dangerous for pregnant women, newborns, and immunocompromised individuals. Nisin's effectiveness against L. monocytogenes underscores its utility in both food safety and clinical settings.
Enterococcus spp.: These bacteria are part of the normal intestinal flora but can cause serious infections in healthcare settings. Nisin's activity against vancomycin-resistant enterococci (VRE) is particularly important given the limited treatment options for these infections.
Potential Applications in Medicine
The unique properties of nisin, particularly its mode of action, make it a promising candidate for various medical applications:
Topical Antimicrobials: Nisin can be formulated into creams, ointments, and gels for the treatment of skin infections, wounds, and burns. Its broad-spectrum activity and safety profile make it suitable for these applications, providing an effective alternative to traditional topical antibiotics.
Respiratory Infections: Inhalable formulations of nisin are being explored for treating respiratory infections, including those caused by antibiotic-resistant bacteria. Direct delivery to the lungs can enhance the efficacy of nisin and reduce systemic side effects.
Gastrointestinal Infections: Oral formulations of nisin have potential for treating gastrointestinal infections caused by pathogens like Clostridium difficile. Nisin's stability in the acidic environment of the stomach and its targeted action in the intestines are advantageous for these applications.
Systemic Infections: While challenging due to potential degradation and rapid clearance from the body, systemic delivery of nisin is being investigated for severe infections. Novel delivery systems, such as encapsulation in nanoparticles, are being developed to overcome these challenges.
Medical Devices and Coatings: Nisin can be incorporated into coatings for medical devices, such as catheters and implants, to prevent bacterial colonization and biofilm formation. This application could significantly reduce the incidence of device-related infections.
Challenges and Considerations
Despite its promising potential, several challenges need to be addressed to fully realize the medical applications of nisin:
Stability and Bioavailability: Nisin can be susceptible to degradation by proteolytic enzymes, limiting its effectiveness in systemic applications. Enhancing its stability and bioavailability is crucial for its therapeutic use.
Delivery Systems: Effective delivery systems are essential for the success of nisin-based therapies. Research is ongoing to develop encapsulation methods and carriers that protect nisin and facilitate its targeted release at infection sites.
Resistance Development: Although resistance to nisin is relatively rare, it remains a concern. Continuous monitoring and the development of strategies to mitigate resistance are essential for the long-term success of nisin-based antibiotics.
Regulatory Approval: Obtaining regulatory approval for new antibiotic formulations involves rigorous testing and validation. Ensuring that nisin-based antibiotics meet the necessary safety and efficacy standards is a complex and time-consuming process.
Cost and Scalability: The production costs of nisin and its derivatives can be high, potentially limiting their widespread use. Advances in biotechnological production methods are needed to reduce costs and enable large-scale manufacturing.
Future Prospects
The future of nisin in antibiotic development looks promising, with ongoing research and technological advancements poised to enhance its applications and effectiveness. Key areas of focus for future development include:
Enhanced Engineering and Design: Continued efforts in genetic engineering and synthetic biology could lead to the development of nisin variants with superior properties, including increased stability, broader spectrum activity, and reduced resistance potential.
Advanced Delivery Systems: Innovative delivery systems that enhance the stability, bioavailability, and targeted release of nisin are critical for its success as a therapeutic agent. Research in nanotechnology, biomaterials, and drug delivery mechanisms will play a vital role in this area.
Combinatorial Approaches: Combining nisin with other antibiotics, antimicrobials, or adjuvants could yield powerful therapeutic regimens that are more effective than monotherapies. Identifying the most effective combinations and optimizing dosing strategies will be important.
Clinical Validation: Conducting comprehensive clinical trials to evaluate the safety and efficacy of nisin-based antibiotics in various settings is essential. Positive outcomes from these trials could pave the way for regulatory approval and widespread clinical use.
Global Collaboration: Addressing the global challenge of antibiotic resistance requires collaboration between researchers, healthcare providers, regulatory agencies, and industry stakeholders. Coordinated efforts can accelerate the development and deployment of nisin-based antibiotics.
Conclusion
Nisin's unique mode of action—disrupting bacterial cell wall synthesis—sets it apart from traditional antibiotics and offers a promising solution to the growing problem of antibiotic resistance. Its broad-spectrum activity, safety profile, and potential for various medical applications underscore its value as a candidate for new antibiotic development. While challenges such as stability, delivery, and resistance development remain, ongoing research and technological advancements hold great potential for overcoming these obstacles. As the search for effective new antibiotics continues, nisin stands out as a valuable and innovative approach, offering hope in the fight against some of the most formidable bacterial pathogens.
- Tel:+8618231198596
- Whatsapp:18231198596
- Chat With Skype







