Tel:+8618231198596

News
 CONTACT
CONTACT
 CONTACT
CONTACT
- Linkman:Linda Yao
- Tel: +8618231198596
- Email:linda.yao@dcpharma.cn
- Linkman:CHARLES.WANG
- Department:Overseas
- Tel: 0086 0311-85537378 0086 0311-85539701
News
Nisin's ability to target specific bacteria reduces the risk of antibiotic resistance development.
TIME:2024-04-01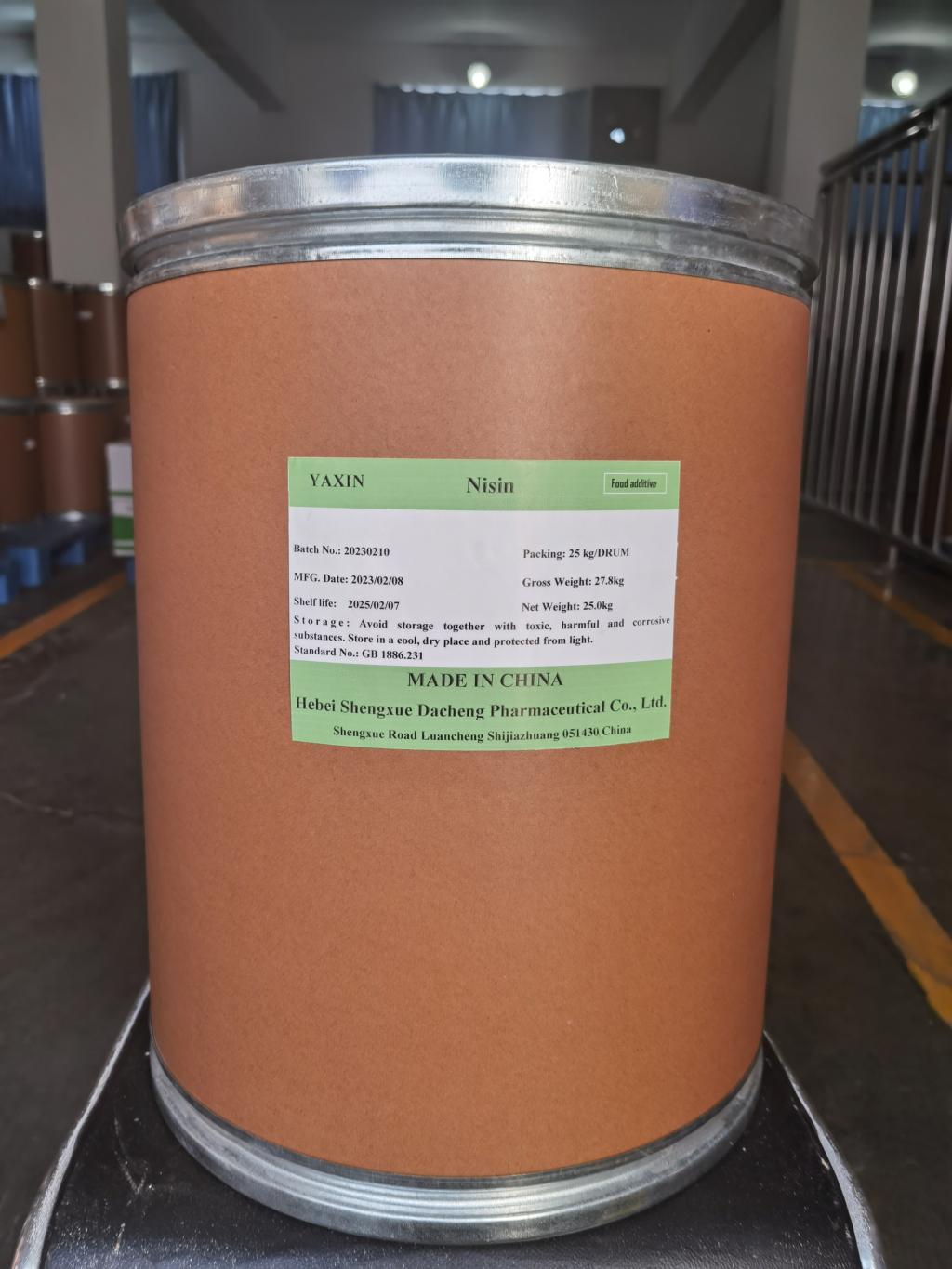
Antibiotic Resistance: A Growing Concern:
Antibiotics revolutionized medicine by enabling the effective treatment of bacterial infections. However, overuse and misuse of antibiotics have accelerated the development of resistance among pathogenic bacteria. Antibiotic-resistant strains render conventional antibiotics ineffective, leading to prolonged illness, increased healthcare costs, and higher mortality rates. The urgent need for alternative antimicrobial strategies necessitates exploring novel agents such as nisin.
Nisin: Nature's Antimicrobial Weapon:
Nisin is a bacteriocin produced by certain strains of lactic acid bacteria, notably Lactococcus lactis. It is characterized by its cationic nature and amphiphilic structure, allowing it to interact with bacterial membranes selectively. Nisin exerts its antimicrobial activity primarily by disrupting the integrity of the bacterial cell membrane, leading to leakage of cellular contents and eventual cell death. Importantly, nisin exhibits specificity towards Gram-positive bacteria while sparing Gram-negative bacteria, which possess an outer membrane barrier.
Mechanisms of Nisin's Targeted Activity:
The targeted antimicrobial activity of nisin stems from its unique mode of action, which involves specific interactions with lipid II, a precursor molecule involved in bacterial cell wall synthesis. Nisin binds to lipid II, forming pores in the cell membrane and disrupting cell wall formation, particularly in susceptible Gram-positive bacteria. This targeted mechanism limits the potential for resistance development, as it relies on bacterial structures essential for growth and survival.
Reduced Risk of Cross-Resistance:
Unlike conventional antibiotics that target specific cellular processes or metabolic pathways, nisin's mode of action targets fundamental components of bacterial cell structure. As a result, the risk of cross-resistance between nisin and conventional antibiotics is minimal. Bacteria must undergo significant genetic changes to develop resistance to nisin, making it a valuable addition to the antimicrobial arsenal, especially in the context of multidrug-resistant pathogens.
Synergistic Interactions with Conventional Antibiotics:
Nisin's ability to enhance the activity of conventional antibiotics through synergistic interactions further underscores its potential in combating antibiotic resistance. Studies have demonstrated synergism between nisin and various antibiotics, including penicillin, vancomycin, and gentamicin, against both Gram-positive and Gram-negative bacteria. By sensitizing bacterial cells to conventional antibiotics, nisin can lower the effective dosage required, thereby reducing selective pressure for resistance development.
Regulatory Considerations and Commercial Applications:
Nisin has a long history of safe use as a food preservative and is approved for use in many countries worldwide. Its regulatory approval and Generally Recognized as Safe (GRAS) status make it an attractive candidate for applications beyond food preservation, including pharmaceuticals, cosmetics, and agricultural products. Commercial formulations of nisin are available in various formats, including liquid, powder, and encapsulated forms, facilitating its incorporation into diverse products.
Future Directions and Challenges:
Despite its potential, several challenges remain in harnessing nisin's full antimicrobial capabilities. These include optimizing production processes to increase yield and purity, elucidating mechanisms of resistance to nisin, and exploring novel delivery systems to enhance efficacy. Additionally, further research is needed to evaluate the long-term effects of nisin use on microbial ecosystems and human health.
Conclusion:
Nisin's ability to target specific bacteria while minimizing the risk of resistance development represents a promising strategy in the fight against antibiotic resistance. Its targeted mode of action, reduced likelihood of cross-resistance, and synergistic interactions with conventional antibiotics position it as a valuable adjunct to current antimicrobial therapies. Continued research and innovation in nisin-based interventions hold the potential to mitigate the global threat of antibiotic resistance and safeguard public health for future generations.
- Tel:+8618231198596
- Whatsapp:18231198596
- Chat With Skype







