Tel:+8618231198596

News
 CONTACT
CONTACT
 CONTACT
CONTACT
- Linkman:Linda Yao
- Tel: +8618231198596
- Email:linda.yao@dcpharma.cn
- Linkman:CHARLES.WANG
- Department:Overseas
- Tel: 0086 0311-85537378 0086 0311-85539701
News
Current Position:
Home >
News
>Nisin: A Rising Star in the Fight Against Hospital-Acquired Infections.
Nisin: A Rising Star in the Fight Against Hospital-Acquired Infections.
TIME:2023-09-22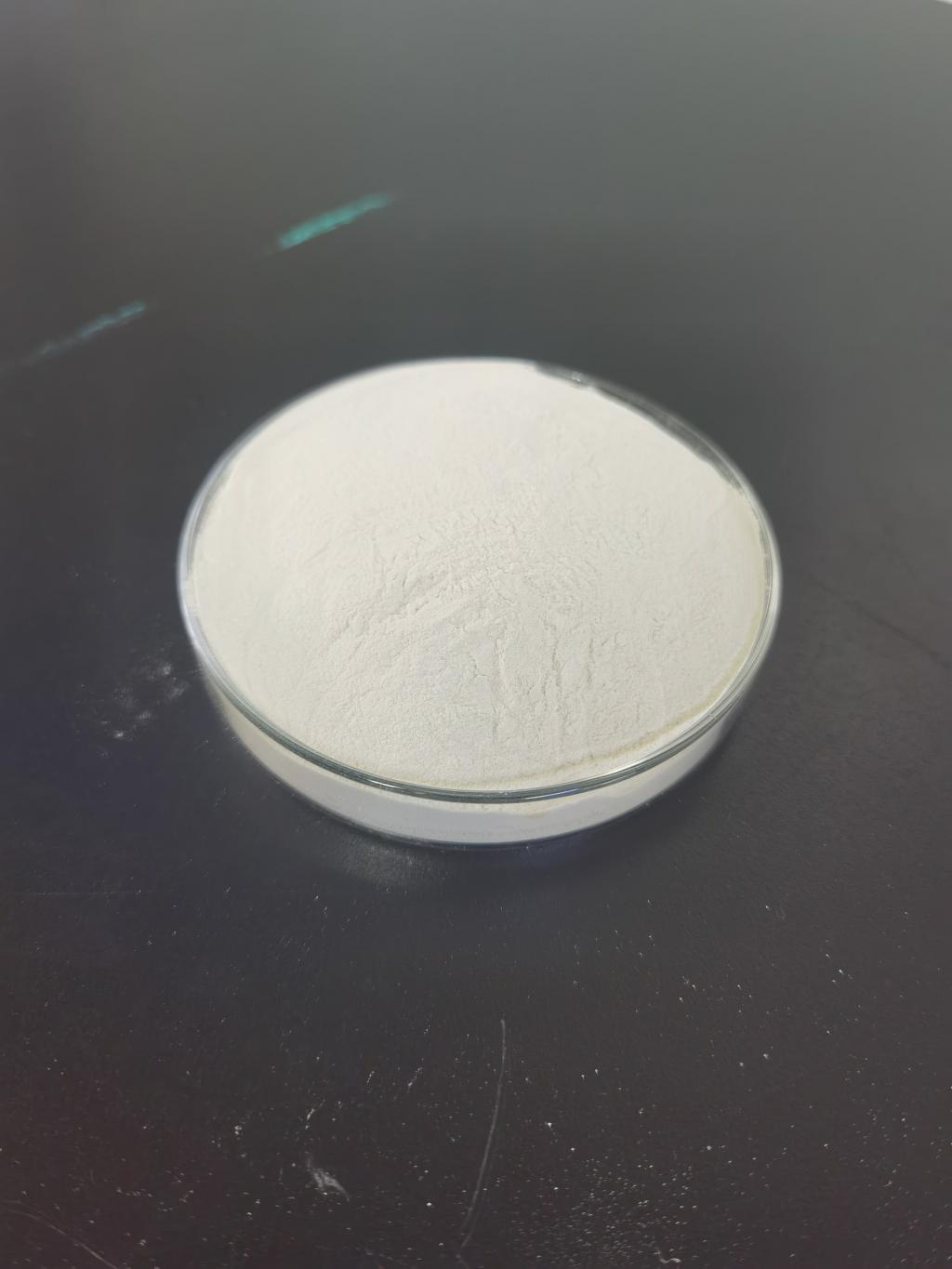
Hospital-Acquired Infections: A Growing Concern
Hospital-acquired infections, also known as nosocomial infections, are infections that patients acquire while receiving medical treatment in healthcare facilities. These infections can occur in various hospital settings, including surgical wards, intensive care units (ICUs), and long-term care facilities. HAIs are a growing concern for several reasons:
a. Antibiotic Resistance: Many HAIs are caused by bacteria that have developed resistance to multiple antibiotics, making treatment challenging.
b. Increased Mortality: HAIs can lead to severe complications and, in some cases, death, particularly in immunocompromised patients.
c. Extended Hospital Stays: Patients who develop HAIs often require longer hospital stays, placing additional strain on healthcare resources.
d. Economic Burden: The economic burden of HAIs includes increased healthcare costs, longer hospitalizations, and lost productivity.
Nisin: Nature's Antimicrobial Peptide
Nisin is a natural antimicrobial peptide produced by certain strains of lactic acid bacteria, notably Lactococcus lactis. It was first discovered in the early 20th century and has since gained recognition for its potent antimicrobial properties. Nisin's unique attributes make it a valuable tool in the fight against HAIs:
a. Broad-Spectrum Activity: Nisin exhibits broad-spectrum antimicrobial activity against a wide range of bacteria, including Gram-positive pathogens such as Staphylococcus aureus and Streptococcus pneumoniae.
b. Safety Profile: Nisin has been deemed safe for human consumption and has generally recognized as safe (GRAS) status from regulatory agencies like the FDA, making it suitable for use in medical applications.
c. Resistance is Rare: Bacteria have shown limited ability to develop resistance to nisin, reducing the risk of resistance-associated treatment failures.
Mechanisms of Action
Nisin's effectiveness against bacteria is attributed to its unique mechanisms of action:
a. Disruption of Cell Membranes: Nisin binds to lipid II, a crucial precursor in bacterial cell wall synthesis. This binding disrupts the integrity of the bacterial cell membrane, leading to cell lysis and bacterial death.
b. Pore Formation: Nisin forms pores in the bacterial cell membrane, allowing the leakage of essential ions and molecules, further disrupting bacterial function.
c. Synergy with Antibiotics: Nisin has shown synergy with various antibiotics, enhancing their effectiveness against drug-resistant bacteria.
Applications in Healthcare Settings
Nisin's potential in healthcare settings extends to various applications:
a. Surface Disinfection: Nisin-based disinfectants and coatings can be used on hospital surfaces, medical equipment, and textiles to reduce bacterial contamination.
b. Surgical Site Infections: Nisin can be incorporated into wound dressings and surgical materials to reduce the risk of surgical site infections.
c. Catheter-Associated Infections: Nisin-coated catheters and urinary devices can prevent catheter-associated urinary tract infections (CAUTIs).
d. Ventilator-Associated Pneumonia: Nisin-coated endotracheal tubes can reduce the risk of ventilator-associated pneumonia (VAP).
Nisin's Role in Combating Multidrug-Resistant Pathogens
Multidrug-resistant (MDR) pathogens, including Methicillin-resistant Staphylococcus aureus (MRSA) and Vancomycin-resistant Enterococci (VRE), have become a major concern in healthcare settings. Nisin offers a promising solution for combating MDR pathogens:
a. MRSA Infections: Nisin has shown effectiveness against MRSA, including strains resistant to conventional antibiotics.
b. VRE Infections: Nisin has exhibited activity against VRE, making it a potential treatment option for VRE-related infections.
c. Biofilm Disruption: Nisin can disrupt bacterial biofilms, which are often associated with antibiotic resistance and persistent infections.
Clinical Trials and Research
The potential of nisin in combating HAIs has garnered significant attention in recent years. Several studies and clinical trials have been conducted or are underway to explore its efficacy and safety in clinical settings. These efforts aim to provide evidence-based support for nisin's role in HAI prevention and treatment.
Challenges and Future Directions
While nisin holds promise in the fight against HAIs, several challenges and considerations must be addressed:
a. Clinical Validation: More extensive clinical trials are needed to establish the efficacy of nisin in various healthcare settings and against specific HAI-causing pathogens.
b. Regulatory Approval: Nisin-based therapies and products require regulatory approval before widespread use in healthcare settings.
c. Cost-effectiveness: The cost-effectiveness of nisin-based interventions compared to existing treatments must be evaluated.
d. Integration into Healthcare Protocols: Healthcare institutions need to adapt their infection control protocols to incorporate nisin-based interventions effectively.
e. Combination Therapies: The potential for combining nisin with existing antibiotics and treatments to enhance efficacy and combat resistance should be explored.
Conclusion
Hospital-acquired infections represent a significant challenge in healthcare, threatening patient safety and increasing healthcare costs. Nisin, a natural antimicrobial peptide with potent broad-spectrum activity and a low risk of resistance development, offers a promising avenue for addressing this issue. Its mechanisms of action, safety profile, and potential to combat multidrug-resistant pathogens make it a rising star in the fight against HAIs. As research and clinical trials continue to shed light on nisin's efficacy and safety, we can anticipate its integration into healthcare protocols and the emergence of new strategies for preventing and treating hospital-acquired infections, ultimately improving patient outcomes and reducing the burden on healthcare systems.
- Tel:+8618231198596
- Whatsapp:18231198596
- Chat With Skype







