
 CONTACT
CONTACT
- Linkman:Linda Yao
- Tel: +8618231198596
- Email:linda.yao@dcpharma.cn
- Linkman:CHARLES.WANG
- Department:Overseas
- Tel: 0086 0311-85537378 0086 0311-85539701
ε-Polylysine Hydrochloride: A Potential Agent for Combating Hospital Biofilm Contamination.
TIME:2024-07-12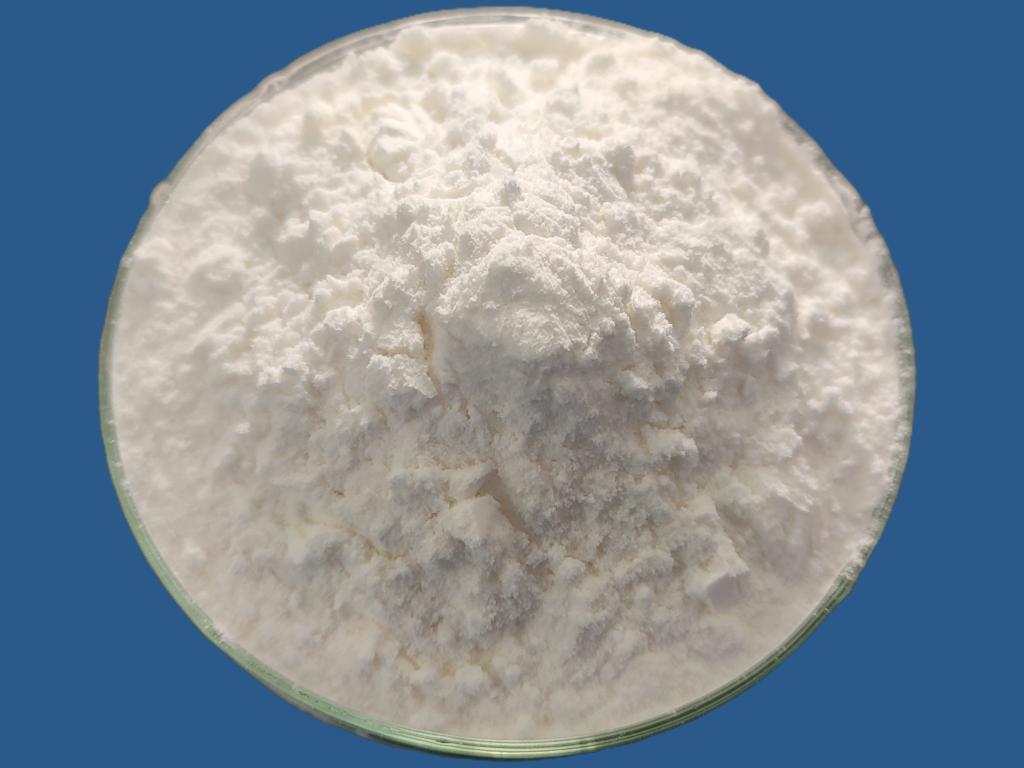
Biofilms are structured communities of microorganisms embedded within a self-produced matrix of extracellular polymeric substances (EPS). These biofilms adhere to surfaces, including medical devices and hospital infrastructure, posing significant challenges in healthcare settings. Hospital-acquired infections (HAIs) associated with biofilms contribute to increased morbidity, mortality, and healthcare costs. ε-Polylysine hydrochloride (ε-PL), a natural antimicrobial peptide, has garnered attention for its potential as an agent to combat biofilm formation and contamination in hospitals. This article explores the mechanisms, applications, current research findings, and future prospects of ε-PL in addressing biofilm-associated challenges in healthcare environments.
Understanding ε-Polylysine Hydrochloride (ε-PL)
Origin and Characteristics
ε-Polylysine is derived from Streptomyces albulus and consists of multiple lysine residues linked by peptide bonds. It is widely recognized for its antimicrobial properties and safety profile in various applications, including food preservation and biomedical settings. ε-PL hydrochloride, the hydrochloride salt form of ε-polylysine, is water-soluble and stable, making it suitable for formulations targeting biofilm-contaminated surfaces in hospitals.
Mechanisms of Action Against Biofilms
Disruption of Biofilm Matrix
ε-PL can disrupt the EPS matrix of biofilms through electrostatic interactions and hydrophobic forces. By destabilizing the structural integrity of biofilms, ε-PL enhances the susceptibility of microbial communities to antimicrobial agents and immune defenses.
Inhibition of Adhesion
ε-PL interferes with microbial adhesion to surfaces by modifying surface properties and inhibiting the initial attachment of microorganisms. This preventive action reduces the formation of biofilms on medical devices and hospital infrastructure, mitigating the risk of HAIs.
Antimicrobial Activity
Beyond its biofilm-disrupting properties, ε-PL exhibits direct antimicrobial activity against a broad spectrum of pathogens, including bacteria and fungi commonly implicated in HAIs. This antimicrobial efficacy contributes to reducing microbial load and preventing biofilm establishment in healthcare environments.
Applications of ε-PL in Hospital Settings
Medical Device Sterilization
Medical devices, such as catheters, implants, and surgical instruments, are susceptible to biofilm contamination. ε-PL-based coatings or disinfectants can be applied to medical surfaces to prevent biofilm formation, enhance sterilization efficacy, and prolong device functionality.
Surface Disinfection
Hospital surfaces, including countertops, bed rails, and equipment, serve as reservoirs for microbial colonization and biofilm formation. ε-PL formulations can be used as disinfectants or surface coatings to reduce microbial adherence, facilitate cleaning protocols, and maintain hygienic environments.
Wound Care and Dressings
Chronic wounds are prone to biofilm formation, delaying healing and increasing infection risks. ε-PL-containing dressings or topical treatments can inhibit biofilm development, promote wound healing, and prevent secondary infections in patients with compromised skin barriers.
Current Research Findings
In vitro Studies
Laboratory studies have demonstrated the efficacy of ε-PL in inhibiting biofilm formation and eradicating established biofilms of clinically relevant pathogens. Researchers have investigated ε-PL formulations, concentrations, and application methods to optimize antimicrobial and anti-biofilm activities.
In vivo and Clinical Trials
Preliminary in vivo studies and clinical trials are underway to evaluate the safety, efficacy, and feasibility of ε-PL in real-world healthcare settings. These studies aim to validate preclinical findings and establish evidence-based guidelines for incorporating ε-PL into infection control practices.
Multi-Drug Resistant Pathogens
The rise of multidrug-resistant pathogens poses challenges in infection control and treatment efficacy. ε-PL's ability to target biofilm-associated drug-resistant microbes offers a promising strategy to combat antibiotic resistance and enhance therapeutic outcomes in patients with difficult-to-treat infections.
Future Directions and Opportunities
Formulation Development
Future research aims to optimize ε-PL formulations for enhanced stability, bioavailability, and sustained antimicrobial activity in hospital environments. Innovations in nanoparticle technology, controlled release systems, and combination therapies could further enhance ε-PL's efficacy against biofilm-associated pathogens.
Integration with Infection Control Practices
Integrating ε-PL-based interventions into comprehensive infection control strategies is essential for maximizing their impact on reducing HAIs and improving patient safety. Collaborative efforts among healthcare professionals, researchers, and regulatory agencies are needed to develop standardized protocols and guidelines for ε-PL use in healthcare settings.
Environmental Impact and Safety
Assessing the environmental impact and safety of ε-PL-based products is crucial for sustainable implementation in hospital settings. Studies evaluating biodegradation, ecotoxicity, and long-term effects on microbial ecology will inform risk assessment and regulatory considerations for ε-PL applications.
Challenges and Considerations
Regulatory Approval and Adoption
Obtaining regulatory approval for ε-PL-based products requires rigorous evaluation of safety, efficacy, and manufacturing quality. Addressing regulatory requirements and demonstrating compliance with healthcare standards are essential steps in advancing ε-PL from research innovation to clinical implementation.
Resistance Development
Monitoring microbial resistance to ε-PL and developing strategies to prevent resistance emergence are critical for maintaining efficacy and prolonging the lifespan of ε-PL-based interventions in infection control practices.
Cost-effectiveness and Accessibility
Ensuring cost-effectiveness and accessibility of ε-PL-based technologies is essential for widespread adoption in healthcare facilities, particularly in resource-limited settings. Economic feasibility studies and market-driven approaches can facilitate affordability and scalability of ε-PL applications.
Conclusion
ε-Polylysine hydrochloride represents a promising bioactive agent for combating biofilm contamination in hospital settings, addressing the complex challenges associated with HAIs and antimicrobial resistance. By disrupting biofilm matrices, inhibiting microbial adhesion, and exerting antimicrobial effects, ε-PL offers a multifaceted approach to enhancing infection control, promoting patient safety, and improving healthcare outcomes. Ongoing research efforts, clinical validations, and collaborative partnerships are crucial for advancing ε-PL from experimental studies to practical applications in infection prevention and treatment strategies. Through innovation, evidence-based practices, and interdisciplinary cooperation, ε-PL holds potential to mitigate biofilm-related risks and contribute to sustainable healthcare practices globally.
- Tel:+8618231198596
- Whatsapp:18231198596
- Chat With Skype







