Tel:+8618231198596

News
 CONTACT
CONTACT
 CONTACT
CONTACT
- Linkman:Linda Yao
- Tel: +8618231198596
- Email:linda.yao@dcpharma.cn
- Linkman:CHARLES.WANG
- Department:Overseas
- Tel: 0086 0311-85537378 0086 0311-85539701
News
Current Position:
Home >
News
>The future of nisin in personalized medicine includes its potential use.
The future of nisin in personalized medicine includes its potential use.
TIME:2024-09-02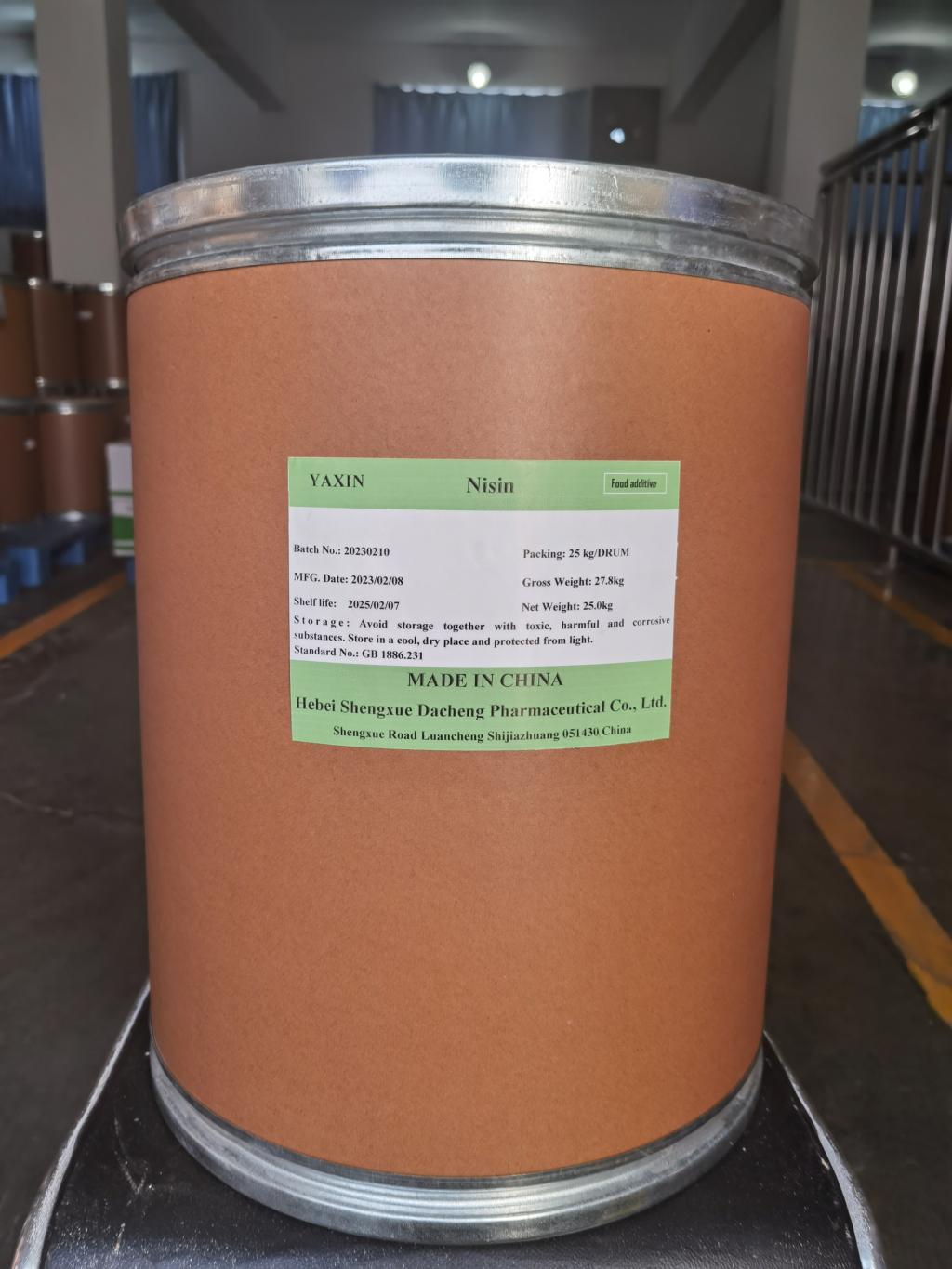
Nisin: A Natural Antimicrobial Agent
Nisin is a lantibiotic produced by the bacterium Lactococcus lactis and is known for its potent antimicrobial activity against a broad range of Gram-positive bacteria. Its mechanism of action involves binding to the lipid II precursor of the bacterial cell wall, leading to the formation of pores and subsequent cell death. This specificity makes nisin an attractive candidate for targeted antimicrobial therapy, particularly in an era where antibiotic resistance is a growing concern.
The Promise of Targeted Antimicrobial Therapies
Traditional broad-spectrum antibiotics, while effective, can disrupt the body's normal flora, leading to secondary infections and contributing to antibiotic resistance. In contrast, targeted therapies aim to selectively eliminate pathogenic bacteria while minimizing disruption to beneficial microorganisms. This approach aligns well with the principles of personalized medicine, which seeks to optimize therapeutic outcomes while reducing side effects.
Nisin in Personalized Medicine
Tailored Treatment Approaches
The use of nisin in personalized medicine could involve identifying patients who would benefit most from its targeted antimicrobial properties. Genetic testing and microbiome analysis can help identify individuals whose infections are caused by nisin-sensitive bacteria. Such personalized approaches could lead to more precise and effective treatments, reducing the likelihood of resistance development and minimizing collateral damage to the patient's microbiota.
Formulation and Delivery
To maximize the therapeutic potential of nisin, researchers are exploring innovative formulation and delivery systems. For instance, nisin can be encapsulated in nanoparticles or conjugated to antibodies that specifically target infected cells. These advanced delivery mechanisms ensure that nisin reaches the site of infection efficiently and in sufficient concentrations, thereby enhancing its efficacy and reducing systemic exposure.
Synergy with Other Therapies
Combining nisin with other antimicrobial agents or immunotherapies could further enhance its therapeutic value. For example, using nisin in conjunction with phages (bacterial viruses) or immunomodulatory drugs could create synergistic effects that improve patient outcomes. This multi-modal approach is particularly relevant in treating complex infections where a single agent might not suffice.
Clinical Applications and Research
While the use of nisin in personalized medicine is still in its nascent stages, several clinical applications are being explored. For instance, topical formulations of nisin are being developed for skin infections, where its antimicrobial properties can be harnessed without systemic absorption. In addition, intravenous or oral forms of nisin are being studied for systemic infections, especially those resistant to conventional antibiotics.
Challenges and Opportunities
Despite the promise of nisin in personalized medicine, several challenges remain. These include optimizing dosing regimens, ensuring the stability of nisin formulations, and addressing potential allergic reactions. Regulatory approval processes for novel antimicrobial agents also need to be navigated. However, the potential benefits of targeted therapies far outweigh these challenges, driving continued research and development efforts.
Conclusion
The integration of nisin into personalized medicine represents a promising frontier in the fight against bacterial infections. By leveraging the specificity and potency of nisin, healthcare providers can tailor treatments to individual patient needs, thereby improving outcomes and reducing the global burden of antimicrobial resistance. As research advances and clinical trials progress, the future of nisin in personalized medicine looks increasingly bright, offering hope for more effective and sustainable therapeutic options.
- Tel:+8618231198596
- Whatsapp:18231198596
- Chat With Skype







